Navigating Flu Season in the COVID-19 Pandemic
November 23, 2020

Since the onset of the pandemic in early March, doctors, researchers and epidemiologists have been concerned with how flu season would challenge doctors in their ability to diagnose whether an illness is flu or COVID-19, as symptoms are very similar.
FLU
What are the differences between flu and COVID-19? The one COVID-19 symptom that is different than flu is a new loss of taste and/or smell. The other symptoms of flu and COVID-19 overlap and include all or some from the list below.
- Fever
- Body aches
- Chills
- Cough, shortness of breath or difficulty breathing
- Headache
- Sore throat
- Runny or stuffy nose
- Fatigue
- Some experience vomiting or diarrhea (most common in children)
“There is so much overlap in the clinical presentation of these two viruses. Physicians with broad experience diagnosing flu and COVID-19 in a variety of patients will prove to be an asset, as will rapid antigen testing,” said Dr. David Gude, Texas MedClinic chief operating officer and practicing physician.
Texas MedClinic, which has 19 urgent care centers spread across San Antonio, Spring Branch, New Braunfels and Austin, has over 35 years under its belt in treating urgent care needs and is usually a first line of defense during flu season. Flu season in the area typically begins in December or January.
From the onset of the COVID-19 pandemic in March, when testing was not widely available, to the present, Texas MedClinic has cared for and tested over 125,000 people of all ages and races with varied degrees of symptoms, including no symptoms at all.
You really begin to understand the disease when you have the opportunity to serve a vast array of patients,” said Gude. “There is only one distinguishing symptom of COVID-19 that is different than flu, and that’s a new loss of taste or smell. That’s why rapid antigen testing can be beneficial. You can test and receive results in 15 minutes, providing clarity and guidance to patients on quarantining and isolation to curb the spread of COVID-19, and providing treatment to those with flu.”
Texas MedClinic patients benefit greatly by having access to rapid antigen tests for both flu and COVID-19. Curbside COVID-19 testing, which is only available for those without symptoms, has been offered at all 19 clinics since July and will continue through flu season.
“Once flu season begins, patients will be tested for both flu and COVID-19. We can test for both viruses easily,” said Dr. David Gude, Texas MedClinic Chief Operating Officer. Patients with symptoms will be required to see a doctor.
For Dr. Gude and his physicians and medical staff, a concern is managing a patient who has both flu and COVID-19. “A dual diagnosis of flu and COVID-19 is possible, and it’s something with which we have no experience. It has not been studied in depth because COVID-19 is a new virus. We do know that contracting multiple diseases or viruses can take a toll on the immune system, worsening symptoms and impairing recovery. We will be paying particularly close attention to this group of patients.”
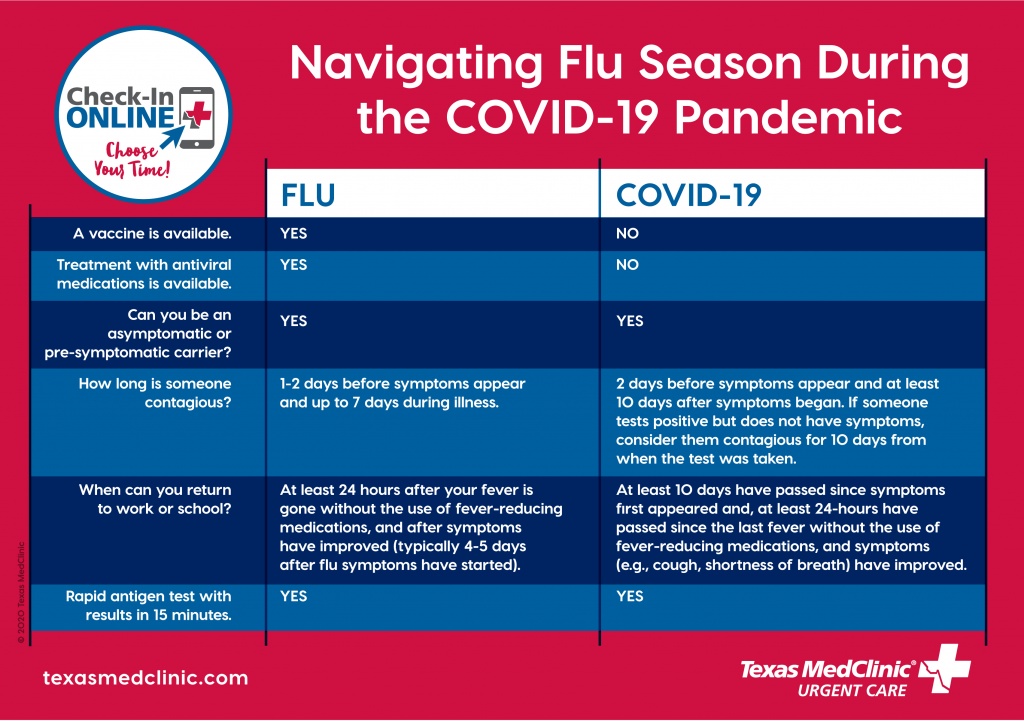
But even with the symptom similarities between flu and SARS-2-CoV, the virus that causes COVID-19, there are other key factors that are different.
Exposure and when symptoms begin
The time it takes for flu symptoms to appear after being exposed to the virus is usually one to two days, but for COVID-19, the time from exposure to symptom onset is 5 to 14 days.
Both flu and COVID-19 are respiratory viruses spread through droplets from sneezing, coughing and talking. Most people with flu are contagious one day before they show symptoms and up to seven days during their illness.
For those with COVID-19, it’s possible to spread the virus for about 2 days before experiencing signs or symptoms and remain contagious for up to 10 days after signs or symptoms first appeared. If someone is asymptomatic, it’s possible to remain contagious for 10 days after testing positive for COVID-19.
“That’s one of the things that makes COVID-19 challenging to manage and control. People have the virus and don’t know they have it because they do not have symptoms and thus can spread the virus exponentially, significantly impacting those who are at a higher risk of severe illness,” said Dr. Gude.
People at high-risk for severe illness
Those who are 65 years and older, those who are pregnant and those with underlying health conditions like diabetes, heart disease or lung conditions like asthma or COPD have a greater risk of complications from contracting flu or COVID-19. Studies have also shown that COVID-19 is more prevalent and the disease more severe in Black and Latino populations.
But data from the last six months suggests that thus far COVID-19 has a minimal impact on children. In contrast, some years and some strains of flu pose a higher risk of severe illness in children.
“Children between the ages of two and five are generally considered at greater risk of the flu worsening into pneumonia or inflamed lungs, as well as an increased risk of dehydration, which can cause serious complications,” said Dr. Gude.
People can reduce the spread of either virus and protect children and those at higher risk of complications from flu or COVID-19 by wearing face coverings or masks, washing hands frequently for at least 20 seconds and maintaining a social distance of at least six feet.
“The flu shot is one of the best ways to protect yourself and your loved ones. There are minimal side effects from the flu shot, and it is widely available and inexpensive,” said Dr. Gude. “And to debunk a myth that has become a popular belief, the flu shot does not give you the flu.”
Treatment for flu or COVID-19
Currently, there is not a vaccine for COVID-19, although researchers and manufacturers are working hard to develop one.
The only COVID-19 treatment options available are for those with severe disease that require hospitalization, as doctors are continuing to learn what therapies and medications are the most effective. There are no outpatient treatments or medications for COVID-19.
However, flu treatment is widely available through time-tested antiviral medications approved by the Food and Drug Administration.
“Tamiflu and Xofluza (two available antiviral medications) attack the flu virus to keep it from multiplying in the body. It is important for those who are experiencing flu-like symptoms to go to their doctor promptly to be tested and diagnosed, as antiviral medications have shown to be effective when taken less than 48 hours from the onset of symptoms,” said Dr. Gude.
When to get tested for flu or COVID-19
Rapid antigen testing provides accurate, fast results for both flu and COVID-19.
The test requires a simple nose swab that can be performed by the patient or parent and takes about 15 minutes to process results.
“For those experiencing flu or COVID-19 symptoms, it’s best to get tested within the first day or two of when those symptoms began,” said Dr. Gude. “For those who have had exposure to COVID-19 but are not experiencing symptoms, it’s best to wait until four or five days post-exposure.”




